Impact Stories
Treating Tuberculosis, the traditional way
Thursday, July 6, 2023
By Elizabeth Mumbi Kigondu
Background
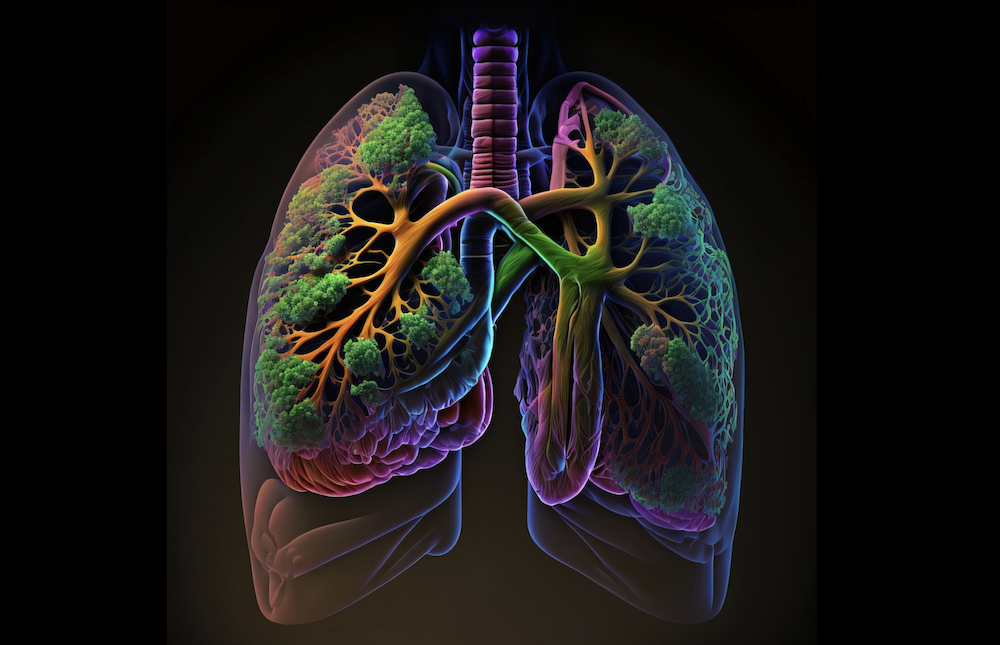
Tuberculosis (TB), an infectious disease, is a leading cause of death worldwide and a persistent global health challenge. In 2021, there were approximately 10.6 million new cases of TB globally, with the disease claiming more than a million lives, according to the WHO. Angola, Bangladesh, and Brazil are the most endemic, followed by other countries including China, India and Ethiopia. Kenya is the tenth highest TB-burdened country. Of those worldwide who live with both the human immunodeficiency virus (HIV) and TB, approximately 80% are in Africa. According to a 2016 survey conducted by the U.S. National Institutes of Health, the prevalence of TB in Kenya is about 558 per 100,000 adults.
Rapidly emerging multi-drug resistant (MDR) and extensively drug-resistant (XDR) strains of Mycobacterium tuberculosis (Mtb), the causative agent of tuberculosis (TB) disease, have hampered TB control in resource-poor countries such as Kenya. This has inspired my current work to search for bioactive molecules that can bypass the development of drug resistance in Mtb.
Multiple factors continue to undermine TB control measures in endemic areas. During the COVID-19 pandemic, low reporting of TB cases led to a rise in cases due to an increase in the number of people with undiagnosed and untreated TB. Other factors that lead to an increase in TB morbidity are the emergence of drug-resistant strains, variable availability and inconsistent quality of frontline anti-TB drugs and prevalence of other chronic diseases. Moreover, the range of effective drugs available for the treatment of MDR-TB is limited, with a few having been developed only in recent years, such as bedaquiline, delamanid and pretomanid. Further, numerous sociological confounders have interfered with efforts to keep TB at bay, such as global socioeconomic inequalities, high levels of population mobility, and rapid urbanization and population growth.
Mtb can cope with the numerous environments it encounters in the course of a successful infection. One way is through its ability to efflux drugs out of the cell with the use of efflux pumps which are localized on the cell membrane of the mycobacterium. There is therefore a dire need to develop novel therapies, especially those that augment the activity of TB drugs in current use, by targeting Mtb’s resistance mechanism. The development of new drugs for the treatment of TB will reduce the chance of the development of resistant strains of Mtb and consequently reduce the number of deaths of TB patients globally, especially in Africa where the TB burden is the greatest.
Approach
The use of herbal products for primary healthcare continues to rise worldwide, with WHO reporting that 80% of herbal product use is in Africa. Many approved drugs used to treat cancer (vinblastine and vincristine), malaria (quinine and artemisinin) and microbial infections (antibiotics such as penicillin, rifampicin, streptomycin) are derived from natural sources such as plants and bacteria. Our study seeks to identify compounds, particularly natural products and their derivatives, that target mycobacteria efflux pumps. We anticipate that inhibition of efflux activity would lead to the accumulation of the anti-TB drug in the mycobacterium cell accelerating clearance of Mtb. The use of natural/herbal products will mean that there are fewer anti-TB drugs required reducing the treatment period and toxicity caused by high concentrations of chemical drugs.
Computational simulations, known as molecular docking studies, are being performed in this project. Seven natural product-based compounds were identified as known Mtb efflux pump inhibitors (EPIs) with good binding affinities and desirable physicochemical properties. Screening of the identified compounds in combination with some anti-TB drugs is ongoing. We’re optimistic that our approach will lead to the identification of compounds that can enhance the biological activity of the current or newly developed anti-TB drugs by blocking the development of resistance and will lead to further pre-clinical and clinical development.
This research is conducted at the Center for Traditional Medicine & Drug Research (CTMDR) and the Center for Respiratory Diseases Research (CRDR) at the Kenya Medical Research Institute (KEMRI) in Nairobi. Our co-principal investigator, Dr Edwin Murungi, a bioinformatician, is based at Kisii University in the Western part of the country. His contribution has been mainly to set up a computational unit at CTMDR to conduct docking experiments. With his expertise, we have also been able to train and mentor two young scientists who are now looking to start their post-graduate studies in computer-aided drug design (CADD).
During this funding period, I was awarded a Scientific Discovery Fellowship by Janssen Pharmaceutical N.V, in partnership with the Johnson & Johnson Foundation. This mentorship programme culminated in a three-month visit to the Janssen labs in Beerse, Belgium, where I was exposed to anti-TB drug discovery projects and I had an opportunity to establish a collaboration with Janssen investigators, who have provided much ongoing support that benefits my current GC-Africa funded project.
I have also been fortunate to receive additional funding from the Medical Research Foundation (MRF) through a Dorothy Temple Cross Tuberculosis International Collaboration Grant. Through this funding, a new collaboration has been established with a team from the University of Bristol led by Dr Paul Race to support our natural products research work.
The H3D Drug Discovery and Development Center at the University of Cape Town has also offered valuable guidance and leadership, recently hosting one of our MSc. students attached to my GC Africa-funded project for a six-week training experience. This opportunity has further strengthened the skills and knowledge of our team that will contribute to achieving our research goals.
Lessons
Among the many lessons learned during this funding period includes the reinforcement of our belief that partnerships and collaborations are key to achieving study objectives, especially for drug discovery. Capacity-building is key, increasing the capabilities of the research group and chances of success. Infrastructure such as research facilities and efficient systems is also a critical success factor. Project management skills and teamwork must underline all our activities for us to achieve our study goals.
About the Author
Elizabeth Kigondu is a grantee of the Grand Challenges Africa programme managed by the SFA Foundation. Kigondu identifies compounds in natural/herbal products and derivates to try and treat drug-resistant TB.
The SFA Foundation's Grand Challenges Africa (GC Africa) programme seeks to promote Africa-led scientific innovations to help countries better achieve the Sustainable Development Goals by awarding seed and scale-up grants to the continent’s most impressive solutions.
Read more about Kigondu's work : https://gcgh.grandchallenges.org/grant/identification-novel-synthetic-and-natural-product-semi-synthetic-derivatives-targeting